As prescription drug costs continue to squeeze state budgets005 Archives a group of state health policy makers is offering some novel — and also some familiar — suggestions for coping. These include regulating the pharmaceutical industry as a utility, allowing states to operate as pharmacy benefit managers and waiving some provisions of the Medicaid program.
In a paper released on Tuesday, the National Academy for State Health Policy also recommends that states pursue laws that require more transparency from drug makers. And the organization floated some timeworn proposals, such as importing medicines from Canada and prosecuting drug makers for violating consumer protection laws that protect against predatory pricing monopolies.
“States, as large drug purchasers, generally negotiate discounts against those high launch prices and against annual price increases, but they are powerless to change the trajectory of the industry pricing model,” according to a paper written by a working group of state legislative staffers, Medicaid programs, state-based insurance exchanges, corrections departments, and attorneys general staffs.
This Tweet is currently unavailable. It might be loading or has been removed.
The proposals come as rising drug costs have sparked outrage and become a talking point in the president campaign. The concern has extended to high prices for new drugs for hard-to-treat diseases, such as hepatitis C and cancer, to continual price hikes for some brand-name medicines and some generic drugs, which are traditionally lower-cost alternatives.
“The proposals in this paper require more dialogue, debate, development, and experimentation. These policy proposals may not be appropriate for all states or agencies, nor for every pharmaceutical product,” the working group wrote. “But states need to act and this paper presents a toolbox of options to consider.”
There is no particular ranking of the 11 proposals made, but at the top of the list is transparency, an issue that has emerged in state legislation around the country. The bills would require drug makers to justify price hikes when prices rise above a certain threshold, or provide breakdowns of their various costs for certain medicines. Only Vermont, however, has passed such a bill into law.
The working group acknowledged the approach has limits: “It may be more useful for states to require pricing documentation, such as a manufacturer’s analyses of what the market will bear, given its current and anticipated product competition, for select high-priced drugs. Manufacturers will no doubt argue that this information is proprietary. However, launch prices are public, and how manufacturers arrive at these prices may be less proprietary than data on drug-specific spending for R&D or marketing.”
So how could states win transparency from drug makers? The working group suggests imposing confidential reporting requirements to obtain the net prices charged to state payers, such as Medicaid managed care plans; rebates offered to pharmacy benefits managers in the state; and savings passed on to other providers, such as hospitals, that participate in a federal program called 340B and receive drugs at discounts.
This Tweet is currently unavailable. It might be loading or has been removed.
Perhaps one of the most contentious proposals, however, is to regulate the pharmaceutical industry as a public utility. The working groups suggests states could create a board to “review, approve, or adjust launch prices for all newly approved drugs, or drugs with list prices above a certain threshold,” as well as price hikes for any drug that exceeds a certain threshold. Open hearings could be held to review data submitted by drug makers and collect other publicly available information.
“Legally, states have considerable discretion to exercise their police power to protect consumers of essential goods and services in markets that do not operate well or rely on a monopoly supplier. Prescription drugs are an essential good; they are as necessary to quality of life — and life itself — as water and sanitation,” the working group writes in explaining its thinking.
There are limitations to this approach, as well, so you may want to read more in the report.
Meanwhile, the working group also discusses the idea of issuing certain types of waivers for Medicaid. For instance, waivers would allow states to opt out of the Medicaid rebate provisions while maintaining a drug benefit that is eligible for federal matching funds. “Under this approach, state Medicaid programs would no longer get the mandatory minimum or best-price rebates,” it said. “In exchange, a state’s Medicaid program could more easily join (other) state agencies or even other states to form a pharmacy benefit manager to run a formulary as commercial payers do.”
This Tweet is currently unavailable. It might be loading or has been removed.
In fact, the working group also suggests that states consider becoming pharmacy benefit managers. “Becoming a strong purchaser is potentially a key to gaining leverage in the market. And a state, operating on behalf of its managed care contractors and other health vendors, could bring scale to innovative contracting that is difficult to achieve as a single-contractor,” it writes.
Before you continue, we have an update in the form of a statement from the Pharmaceutical Research & Manufacturers of America, the industry trade group. A spokeswoman wrote us to say that “many of the solutions proposed by the Work Group would harm patients and limit their access to life-saving treatments. We hope to begin a dialogue with the National Academy for State Health Policy on solutions that will help states better manage and predict costs while preserving patient access.
“Cost pressures on Medicaid – and states more broadly – are real and need to be addressed. At the same time, we need to look at these cost drivers holistically and ensure we maintain a health care system that supports patient access to treatments and fosters the development of tomorrow’s treatments and cures to address significant unmet medical needs.”
What else did the working group propose? States can create purchasing pools, although these do not necessarily affect pricing trends and negotiating leverage may be limited. The working group also suggests states achieve an acceptable return on investment and explore value assessments, such as those calculated by the Institute for Clinical and Economic Review, a nonprofit that has irked drug makers.
Yet another suggestion is forward financing strategy, in which risk is removed — a price is negotiated up front, and payment to the drug maker is delayed until a future date. In return, drug makers would gain either market share, market access, or seek to benefit from upside risk. And another proposal involves bulk purchasing in which states could act individually or together.
Previous:White Nationalism’s New Clothes
Next:Fresh Hell
 Control-Alt-Fail
Control-Alt-Fail
 Covid vaccine: Why it's wise to wait two weeks after your shot
Covid vaccine: Why it's wise to wait two weeks after your shot
 Franzen on Kraus: Footnote 48 by Jonathan Franzen
Franzen on Kraus: Footnote 48 by Jonathan Franzen
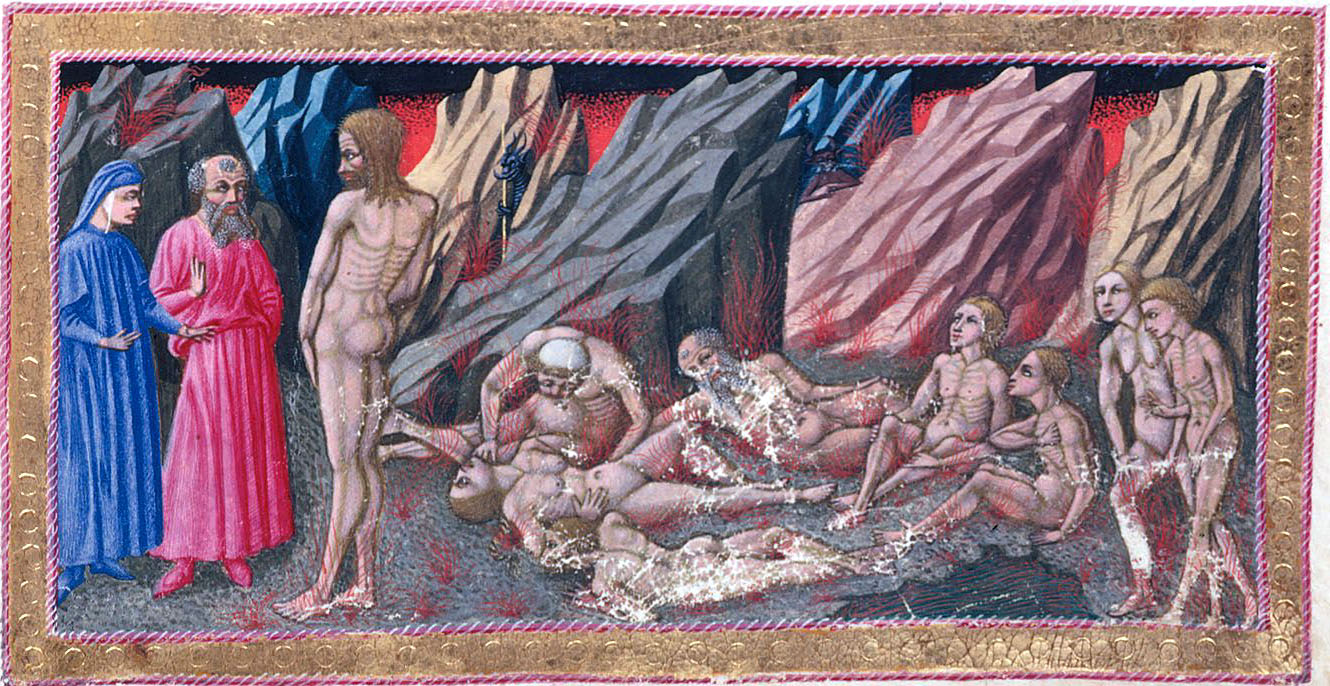 Recap of Canto 14 of Dante’s “Inferno”
Recap of Canto 14 of Dante’s “Inferno”
 The Zuckerberg Follies
The Zuckerberg Follies
 'Barbie': Where to buy Ken's 'I am Kenough' sweatshirt
'Barbie': Where to buy Ken's 'I am Kenough' sweatshirt
 Anthony Cudahy
Anthony Cudahy
 The Morning Roundup for January 16, 2014
The Morning Roundup for January 16, 2014
 A Rich Fable
A Rich Fable
 TikTok launches text posts amidst Twitter 'X' rebrand
TikTok launches text posts amidst Twitter 'X' rebrand
 The Last Line of Defense
The Last Line of Defense
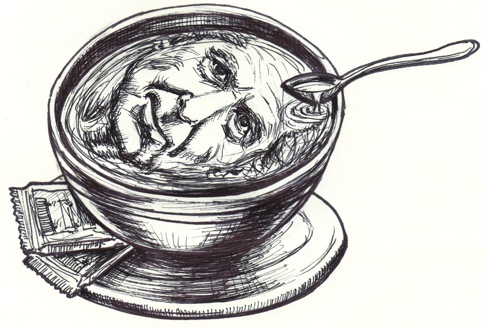 Illustrated author portmanteaux of the two
Illustrated author portmanteaux of the two
 'Barbie': Where to buy Ken's 'I am Kenough' sweatshirt
'Barbie': Where to buy Ken's 'I am Kenough' sweatshirt
 Big Trouble in Little Poland by Sadie Stein
Big Trouble in Little Poland by Sadie Stein
 We Shall Be Terrible
We Shall Be Terrible
 Why did Justin Simien walk the 'Haunted Mansion' red carpet?
Why did Justin Simien walk the 'Haunted Mansion' red carpet?
 The Morning Roundup for January 15, 2014
The Morning Roundup for January 15, 2014
 Siri Hates Her, and Other News
Siri Hates Her, and Other News
 Bafflersplainer: Win the Future
Bafflersplainer: Win the Future
 How to switch to Mastodon from Twitter
How to switch to Mastodon from Twitter
Philly's IToward a More Radical Selfie by India EnnengaBest holiday deal: Buy a preThe best gift for Apple lovers? This ‘Windows Ugly Sweater.’Staff Picks: Sports, Sontag, and Scheherazade by The Paris ReviewNo One Has a Monopoly on DeathI successfully haggled with an AI garage sale by empowering itStaff Picks: Good Guys, Goose Fat, and Ghosts of Mars by The Paris ReviewLeonard Michaels Was a Cat Person by Sigrid NunezBest Shark FlexStyle deal: Save $100 for a limited time via Best Buy DropsThe best gift for Apple lovers? This ‘Windows Ugly Sweater.’Best bird feeder deal: Get the solarPoetry Rx: There’s No Going Home by Claire SchwartzPoetry Rx: You Have Become Everything You Needed To Become by Claire SchwartzLeonard Michaels Was a Cat Person by Sigrid NunezWordle today: The answer and hints for November 28Wordle today: The answer and hints for November 28iPhone trick lets you say 'Next' to scroll through TikTok handsWhat's wrong with my houseplant? Here's how to figure it out.Yan Lianke Illuminates Contemporary China by Carlos Rojas Game of Thrones' star Sophie Turner tweets a powerful thread about mental illness Who's behind the egg that broke the Instagram world record? Uber safety update puts users with non Magical pooch performs tricks to 'Harry Potter' spells, deserves 10 points for Gryffindor U.S. military orders initial batch of Microsoft HoloLens AR goggles Pakistan floods: Here's how you can help. DoorDash data breach leaves important customer details exposed Apple may retire the iPhone mini, but the small iPhone dream lives on Australian woman allegedly received an accidental multimillion Anderson Cooper asked Alexandria Ocasio Macaulay Culkin expertly trolls his little brother on Twitter during the Golden Globes Wordle today: Here's the August 29 Wordle answer and hints Moose casually wanders into hospital on a snack run Woman stuck in airport fights terminal boredom by making a hilarious dance video This flaming cocktail belongs in 'Harry Potter' Sex toy debacle reveals shameful double standard at CES 'Welcome to Wrexham' review: Gripping sports doc, but don't watch it for the celebs The bizarre phenomenon of vacation surprise videos Everything you need to know about THAT 'She 'Wordle' today: Here's the answer, hints for September 2
2.5212s , 8246.65625 kb
Copyright © 2025 Powered by 【2005 Archives】,Information Information Network